U.S. doctors revealed a "detective story" about Rapunzel syndrome.
A case report from a Massachusetts general hospital (USA) was published by the journal New England Journal of Medicine. It indicates that the patient began experiencing periodic abdominal pain approximately one month before seeking medical attention. Initially, the pain occurred every few days but then intensified to twice a day. The young woman also experienced nausea and vomited three times. Due to her condition, she missed school, prompting her parents to take her to the local hospital's emergency department for evaluation.
In discussions with medical staff, the patient described her pain as sharp, rating its intensity at eight out of ten. Following an examination, laboratory tests, and an ultrasound of the abdominal and pelvic organs, which showed no abnormalities, she was sent home. She was advised to take pain relievers, a medication for stomach ulcers, and another drug for nausea and vomiting.
Throughout the following week, her abdominal pain and nausea recurred intermittently. A single dose of ibuprofen did not help — the pain only worsened. Ultimately, she decided to stop using it. She also did not take any of the other prescribed medications.
After one of the pain episodes that occurred at night, her parents took her to the emergency room again, but to a different hospital. The doctors repeated the ultrasound, conducted blood tests, and checked for gonorrhea and chlamydia, but again found no anomalies. The patient was sent home with the same instructions as before — to take an antiemetic, an ulcer medication, and a painkiller.
The young woman returned to the Massachusetts general hospital a week later, as her condition continued to deteriorate. On the day of admission, she vomited five times, and the pain episode lasted for 15 minutes.
Once again, the patient underwent a thorough examination. Her body temperature was normal, blood pressure and pulse were stable, and her abdomen was soft upon palpation. There was no diarrhea. The medical team repeated necessary tests, adding a CT scan, but still could not identify the source of her pain.
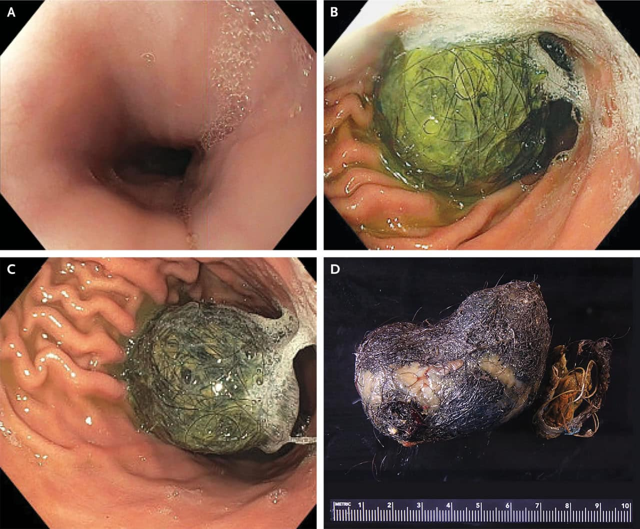
After ruling out obvious pathologies, including constipation, gastritis, delayed gastric emptying due to infection, lactose intolerance, gallbladder diseases, and pancreatitis, the doctors considered rarer conditions. One of the "suspects" was a trichobezoar — a mass of undigested hair in the gastrointestinal tract. On CT images, such formations can be indistinguishable from food in the stomach.
In particularly rare cases, the hair accumulation is so large that its "tail" extends into the intestines. This condition is referred to as Rapunzel syndrome, named after the fairy tale character known for her long hair.
To verify this hypothesis, an esophagogastroduodenoscopy was performed — a visual examination of the upper gastrointestinal tract using an endoscope. As a result, the patient was found to have a trichobezoar approximately seven centimeters wide with a "tail" reaching the small intestine. The hairball was subsequently surgically removed using a gastrostomy tube.
Among the possible causes of trichobezoars are psychological disorders related to pulling, biting, and eating one's own hair (trichotillomania and trichophagia). Given this, the young woman was advised to consult a psychiatrist after her recovery and discharge from the hospital. However, she did not attend her follow-up appointment for outpatient treatment and informed the doctors that she intended to see a hypnotherapist recommended by friends. No further information about her fate has been reported.
It's worth noting that the described case of Rapunzel syndrome is far from the most extreme. Another shocking example was recently reported by Russian doctors. An October publication in the Telegram channel of the Ministry of Health of the Novosibirsk region revealed that local surgeons extracted a trichobezoar measuring 35 x 10 x 8 centimeters and weighing over two kilograms from the stomach of a 19-year-old patient. The doctors found that this outcome was due to the young woman eating her hair for three years.